In the realm of healthcare policy, one term that often arises is “Certificate-of-Need” (CON). This regulatory framework aims to govern the establishment or expansion of healthcare facilities and services. In this blog post, we’ll dive into the concept of Certificate of Need, explore its historical background, and examine its pros and cons.
What Is a Certificate of Need and What Is Its Purpose?
Certificate of Need definition: a CON is a legal document issued by a state or regional regulatory body that grants permission to healthcare providers to initiate new medical facilities, expand existing ones, or introduce certain medical services or technologies within a defined geographic area.
So, certificate of need laws are intended to do what exactly? The primary objective of CON laws is to control healthcare costs, prevent unnecessary duplication of services, and maintain quality care standards.
The History of Certificate of Need Legislation
The roots of Certificate of Need legislation can be traced back to the 1960s, when concerns regarding escalating healthcare costs and surplus healthcare facilities emerged. To address these issues, several states in the United States began implementing CON laws. These laws were predominantly introduced to promote planning, coordination, and efficiency in healthcare delivery by controlling the supply of healthcare services.
Certificate of Needs Law Origins and Federal Mandate
- 1964 – New York leads the way: The first Certificate of Need law was passed in New York to regulate hospital expansions and capital expenditures.
- 1974 – National adoption: Congress passed the National Health Planning and Resources Development Act, requiring states to implement CON laws to qualify for federal funding.
- 1980s – Nearly nationwide: By the early 1980s, almost every state had a certificate of need law in place.
Why States Adopted Certificate of Need Laws
- Cost control: Limit duplication of services and reduce unnecessary spending.
- Quality and access: Ensure specific high-volume or specialized procedures are concentrated in appropriate facilities.
- Planning and coordination: Align healthcare growth with community needs instead of market forces alone.
Federal Repeal and State Responses
- 1987 – Federal repeal: Congress withdrew the national requirement after concerns that CON laws were not achieving their goals.
- State-level decisions: Since then, many states repealed their certificate of need laws, while others kept or modified them. By 2008, 14 states had eliminated their programs.
The Current Status of Certificate of Need Laws by State
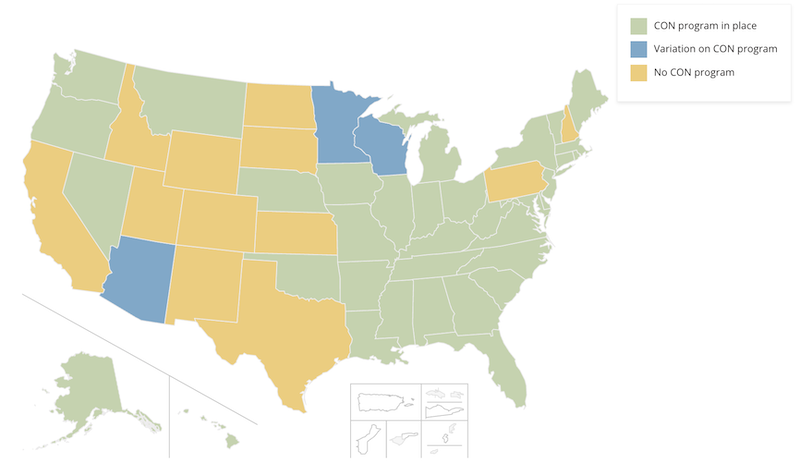
Part of the underlying challenge associated with these laws lies in the fact that they are subject to regulation at the state level, thereby resulting in a lack of uniformity and consistency across different jurisdictions, as each state adheres to its own unique set of processes and requirements.
The impact of the law, however, is quite clear: in states without a Certificate of Need, such as Texas, there are over 450 Medicare-certified surgery centers, and they are thriving. In other states, such as those in the Northeast, growth is slow, complicated, and a headache. Plus, the Kaiser Family Foundation found that states with CON laws had 11% higher healthcare costs than states without those laws.
At a high level:
How Many States Have Certificate of Need Laws?
- 12 states have no program: California, Idaho, Wyoming, Utah, Colorado, New Mexico, Texas, North Dakota, South Dakota, Kansas, Pennsylvania, New Hampshire
- 3 states have some variation of a program: Arizona, Minnesota, and Wisconsin.
- 35 states and have fully intact CON laws: Alabama, Alaska, Arkansas, Connecticut, Delaware, Florida, Georgia, Hawaii, Illinois, Indiana, Iowa, Kentucky, Louisiana, Maine, Maryland, Massachusetts, Michigan, Mississippi, Missouri, Montana, Nebraska, Nevada, New Jersey, New York, North Carolina, Ohio, Oklahoma, Oregon, Rhode Island, South Carolina, Tennessee, Vermont, Virginia, Washington, and West Virginia.
How Do Certificate of Need Laws Change Today and What Is Their Impact?
The surgery center industry is poised for substantial growth in the upcoming years. The increasing trend of payers urging procedures to be performed in outpatient facilities, coupled with advancements in technology that facilitate the performance of more intricate procedures, sets the stage for unprecedented opportunities.
However, the frustration arises when the potential expansion is impeded by Certificate of Need laws. Despite the substantial investments planned by the top five ASC management groups, these restrictive regulations hinder the industry’s potential for growth.
According to the NCSL, in 2022, at least 12 states – Arizona, Connecticut, Kentucky, Louisiana, Maryland, Michigan, Mississippi, New York, Ohio, Oklahoma, Vermont, and Virginia – and Washington D.C., enacted legislation modifying their CON laws in some capacity.
Becker’s ASC Review did a great job of summarizing some of the latest movements and how some management groups are dealing with this situation.
The Current Challenges and Evolution of Certificate of Need Laws
Applying for a Certificate of Need can be a long and expensive process, often taking years and costing hundreds of thousands of dollars in legal and regulatory fees.
A controversial aspect of CON programs is that existing hospitals and healthcare providers can object to new applications. In practice, this means established players can block new competitors by arguing there is “no need” for additional facilities or services. As one think tank famously put it, this is like Burger King having the power to decide whether McDonald’s can open a new restaurant down the street.
Who Benefits from Certificate of Need Laws?
- Incumbent providers: Large hospitals, physician groups, and established healthcare systems gain the most. CON laws protect them from competition by raising barriers to entry.
Who Do CON Laws Harm?
- Patients and taxpayers: Studies show that states with certificate of need laws face higher healthcare costs, fewer hospital beds, and fewer facilities compared to states without these restrictions. For example, research from the Mercatus Center at George Mason University found that states with a CON program have about 30% fewer hospitals per 100,000 residents, along with nearly 99 fewer hospital beds per 100,000 people, compared to non-CON states. These states also tend to have fewer Ambulatory Surgical Centers (ASCs), limiting access to outpatient care.
- Access to care: CON laws are associated with fewer hospitals and Ambulatory Surgical Centers (ASCs). Rural communities are especially impacted, as facilities may be blocked before they can even be built.
- Healthcare costs: The Kaiser Family Foundation found healthcare costs were roughly 11% higher in CON states than in non-CON states.
Temporary Suspensions of Certificate of Need Laws During the Pandemic
During the COVID-19 crisis, 24 states suspended their CON programs to allow hospitals to expand capacity more quickly. Florida, for example, relaxed its CON laws, and new hospitals began opening soon afterward. These suspensions fueled questions about whether CON restrictions are essential.
Certificate of Need Laws’ Recent Developments & Reform Momentum (2023–2025)
A 2024 study found that repealing CON requirements for Ambulatory Surgical Centers (ASCs) led to a 44–47% increase in ASCs overall, and a roughly double (92–112%) increase in rural areas, without leading to hospital closures. Another analysis revealed that more hospitals emerged in both rural and urban settings following the CON repeal, with these hospitals tending to be smaller, suggesting increased competition rather than consolidation.
Moreover, while the core arguments for and against CON laws remain, a clear trend of legislative reform and legal challenges has emerged across the United States. This movement, often driven by free-market advocates and healthcare innovators, seeks to loosen or repeal regulations that they consider anti-competitive.
- South Carolina took the first steps in repealing CON laws in 2023. Governor Henry McMaster signed S. 164, which initiated a phased repeal of the state’s CON laws, rather than an immediate and complete one. The legislation immediately eliminated CON requirements for most health facilities, including ambulatory surgical centers and new hospitals with up to 50 beds in counties lacking a hospital. However, it maintained CON regulations for nursing homes. It established a phased-out repeal for hospitals in counties that already have a hospital, with this portion of the law not taking full effect until January 1, 2027. This reform was enacted to foster greater healthcare competition and improve patient access by lowering barriers for providers to establish or expand services.
- In 2023, North Carolina passed HB 76, adjusting expense thresholds for CON requirements and exempting several facility types, such as chemical dependency and psychiatric centers, from the CON process.
- Following a legal challenge from a mother seeking to open a birthing center, Georgia’s Governor signed a law in 2024 that reformed some of the state’s CON laws. The new legislation aims to reduce regulatory barriers for specific healthcare services, such as birthing centers.
- Also in 2024, Tennessee enacted legislation that incrementally modifies its CON requirements. The law exempts specific services, such as open-heart surgery, burn units, and MRI services, from the need for a CON, while keeping the requirements in place for others. This shows a state-level strategy of targeted deregulation rather than a full repeal.
- New York recently finalized updates to its CON regulations (effective August 6, 2025), loosening review requirements to speed up provider approvals and investment.
- In 2025, Iowa shifted oversight of its CON program from the State Health Facilities Council to the Department of Health and Human Services, centralizing administration under a single agency.
Legal battles against CON laws also constitute a significant development. A prominent case in North Carolina, Singleton v. NC Dept. of Health and Human Services, saw the state Supreme Court in late 2024 allow an eye surgeon’s lawsuit to move forward. The doctor is arguing that the CON law is unconstitutional under the state’s laws against monopolies and exclusive privileges. This case, along with others, highlights how legal challenges are increasingly being used as a tool to dismantle CON regulations on constitutional grounds.
It Isn’t All Bad: Pros of Certificate of Need Laws
In this ongoing debate, it’s crucial to understand the arguments in favor of Certificate of Need CON laws. While critics focus on their potential to stifle competition, proponents argue that these regulations serve a vital role in protecting the healthcare system and ensuring a higher standard of care for the public. The following points highlight the core benefits cited by those who support the continued use of CON laws.
- Cost Control: CON laws are designed to prevent the overinvestment in healthcare infrastructure, which can lead to increased costs. By evaluating the need for new facilities and services, CON laws help avoid unnecessary expenses and promote cost-effective allocation of resources.
- Quality Assurance: The regulatory process of obtaining a Certificate of Need often involves an assessment of the proposed facility or service’s impact on the existing healthcare landscape. This evaluation ensures that new providers meet certain quality standards, helping to maintain and improve the overall quality of care delivered to patients.
- Community Planning: Certificate of Need laws encourage systematic and comprehensive healthcare planning. By requiring healthcare providers to demonstrate the need for their proposed services, CON laws facilitate strategic decision-making, prevent excessive competition, and promote the equitable distribution of resources within a community or region.
As we’ve seen, the arguments in favor of CON laws are compelling on paper, promising a more controlled, efficient, and equitable healthcare system. However, the reality of their implementation often falls short of these ideals, as evidenced by the high-profile repeals and ongoing debates we’ve discussed. The tension between these stated benefits and their real-world consequences is at the heart of the modern CON law debate.
It Isn’t All Good Either: Cons of Certificate of Need Laws
Despite their stated goals of promoting efficiency and quality, the implementation of Certificate of Need laws has faced significant criticism. On the other side of the debate, opponents argue that these regulations are a powerful force for harm, creating unintended negative consequences for competition, costs, and patient access to care. The following points highlight the core arguments against these laws, which have fueled the recent push for their reform and repeal across the country.
- Limited Competition & fewer options: Critics argue that CON laws can stifle competition by creating barriers to entry for new providers. The regulatory process and associated costs can deter smaller healthcare providers or entrepreneurs from entering the market, potentially limiting consumer choice and innovation.
- Delayed Access to Care: The lengthy and complex process of obtaining a Certificate-of-Need can cause delays in the establishment or expansion of healthcare facilities. These delays may hinder timely access to healthcare services, particularly in areas with a shortage of providers or specialized care.
- Inefficiencies and Bureaucracy: Some opponents of CON laws contend that the regulatory process can be burdensome and bureaucratic. The administrative requirements and subjective decision-making involved may introduce inefficiencies, impeding the timely delivery of healthcare services.
- They protect established industry leaders from competition by limiting entry into the health care marketplace. Unlike a free-market system, CON laws harm consumers (aka patients), leading to fewer health care options at higher prices. Moreover, CON stifles innovation, leaving patients with less access to emerging technologies in the medical marketplace.
The critiques of CON laws paint a picture of a regulatory system that, in practice, protects established players at the expense of patients and innovation. The documented impacts are the very reasons many states have chosen to either scale back or eliminate their programs. This deep-seated tension between theoretical benefit and practical harm remains the central conflict in the policy discussion surrounding CON laws.
Certificate of Need Laws and the Future of Healthcare
Certificate-of-Need legislation has been a subject of ongoing debate in the healthcare policy arena. While proponents argue that CON laws help control costs, ensure quality care, and promote community planning, opponents raise concerns about limited competition, delayed access to care, and bureaucratic inefficiencies.
Looking ahead, one of the most promising forces in bridging these gaps is the Ambulatory Surgery Center (ASC) industry. ASCs are uniquely positioned to reduce disparities in care by expanding access to outpatient procedures, lowering costs for patients, and easing the burden on hospitals. In states without restrictive CON laws, the rapid growth of ASCs has demonstrated how innovation and patient-centered models can thrive when regulation allows room for competition.
Striking the right balance will require thoughtful reform, ensuring both affordability and quality while also embracing the role of ASCs in addressing care delivery inequities. If policymakers can align regulation with innovation, the healthcare system will be better equipped to provide accessible, high-quality services for all communities.
Frequently Asked Questions About Certificate of Need Laws
Explore these key questions to gain a deeper understanding of how certificate of need laws operate, their scope, and their impact on healthcare services.
1. What are Certificate of Need laws?
Certificate of Need laws are regulations that require healthcare providers to obtain state approval before building new facilities, expanding services, or purchasing significant medical equipment. These laws aim to align healthcare infrastructure with community needs while preventing unnecessary duplication and controlling costs. CON reviews typically assess factors like projected demand, financial feasibility, and the impact on existing providers.
2. How many states have Certificate of Need laws today?
As of early 2025, 35 states plus Washington, D.C., maintain some form of CON laws. However, the scope and enforcement of these regulations vary widely, which is why it is essential to review Certificate of Need laws by state to understand the differences in requirements and restrictions across the country.
3. How can a healthcare facility get a Certificate of Need?
To obtain a CON, a provider typically follows a structured process:
- Demonstrate “need”, often using population and utilization data or tailored justification.
- Submit a formal application, including details like financial viability and operational impact.
- Notify the public and allow existing providers to raise objections.
- Undergo a review period, which can take months to years, and potentially face appeals or legal challenges.
These requirements vary by state in terms of data format, delegation authority, filing fees, and procedural timelines.
4. Do Certificate of Need laws affect Medicare or Medicaid services?
Yes. While CON laws are state-level regulations, they can also influence Medicare and Medicaid service delivery. Providers seeking reimbursement must still comply with CON requirements before offering services to Medicare or Medicaid patients. This means that even federally funded care is subject to state-approved expansions of facilities or services. In some cases, CON approval is required before adding services such as dialysis, surgical centers, or imaging equipment that serve federally insured populations.
Don’t miss out on the good stuff – Subscribe to HST’s Blog & Podcast!
Every month we’ll email you our newest podcast episodes and articles. No fluff – just helpful content delivered right to your inbox.