Efficient utilization of operating rooms (OR) is crucial for the success of any surgery center. By optimizing block time and following block time best practices, surgery center leaders can uncover a ton of revenue that is currently being left behind.
But, keeping utilization high can be tricky.
In fact, after analyzing data from over 450 ASCs, we determined that, on average, 42% of blocked OR time is unused. Wasted OR time = wasted revenue opportunity.
Here are ten tips to help you achieve better OR utilization through effective management of block time.
1. Pay Close Attention to Historical Utilization Analysis
Understanding past utilization patterns is essential for making informed decisions, so it’s vital that you analyze historical data to identify trends in OR usage. This analysis can help you adjust block time allocations to match actual needs, reducing idle time and ensuring resources are used efficiently.
2. Implement Dynamic Scheduling Systems That Allow Real-Time Adjustments
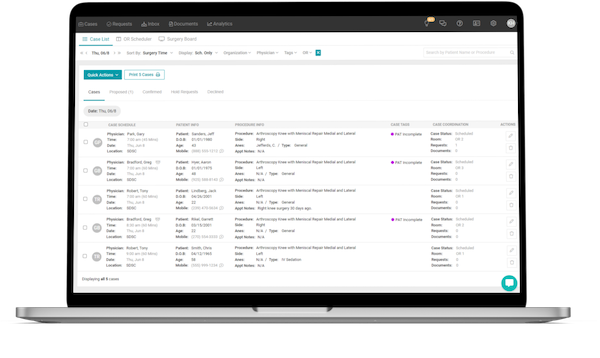
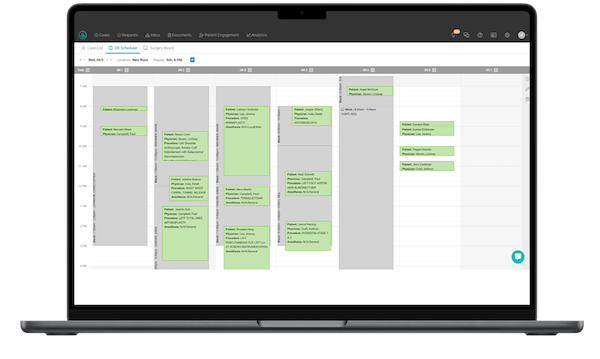
Traditional scheduling systems can be rigid, leading to inefficiencies. Invest in dynamic scheduling systems, such as HST’s scheduling & care communication, that offer real-time adjustments. These systems enable you to quickly reallocate OR time based on cancellations or changes, making sure no time goes to waste and improving overall utilization.
3. Utilize Automated Systems to Remind Providers to Release Unused Block Times
Automated reminders can significantly reduce unused block times. Implement systems that notify providers when they have unused block time approaching, prompting them to release it if they don’t need it. This proactive approach helps maximize OR availability for other providers.
4. Share Open Availability with Providers to Optimize Scheduling
Transparency in scheduling can lead to better utilization. Regularly update and share a schedule of open block times with all providers. This visibility allows providers to plan and request available slots, reducing last-minute scrambles for space. To take it one step further, HST’s scheduling & care communication has many features, such as allowing physician schedulers to request OR time online, making it easy for referring practices to send you more cases.
5. Require Providers to Release Unused Block Times at Least 48 Hours in Advance, Ideally 72 Hours
Establishing a policy that requires providers to release unused block times at least 48 hours in advance, with 72 hours being ideal, will help make sure they are reallocated effectively. This advance notice gives the scheduling team enough time to fill the slots with other cases, optimizing OR usage.
6. Implement Consequences for Late Release
Encourage timely release of block times by implementing consequences for late releases. This could include reduced future block allocations or other administrative actions. By holding providers accountable, you can foster a culture of efficiency and responsibility.
7. Have a Clear and Fair Process for Reallocating Released Block Times to Other Providers
Establish a transparent process for reallocating released block times that is fair and based on a set of clear criteria, such as provider availability and patient needs. Clear guidelines help prevent conflicts and ensure that the reallocation process is smooth and efficient.
8. Publicly Recognize Providers Who Efficiently Use Their Allocated Block Times, Striving for 70% Usage
Recognition can be a powerful motivator. Publicly acknowledge providers who consistently use their allocated block times efficiently, aiming for at least 70% usage. Highlighting their efforts not only rewards them but also sets a benchmark for others to strive towards.
9. Share Reports Correlating Unused Block Time with Budget and Revenue Impacts
Data-driven insights can drive change. Regularly share reports with providers that correlate unused block time with budgetary and revenue impacts. When providers understand the financial implications of unused OR time, they are more likely to release it, improving overall efficiency.
10. Collect and Analyze Data
Continuous improvement requires comprehensive data analysis. Collect and analyze various metrics, including utilization rates, procedure durations, turnover times, provider performance, and patient flow data. If you want to see how you compare to your peers, check out HST’s State of the Industry Report with free benchmarking data.
By implementing these ten tips, surgery center leaders can significantly improve OR utilization. If you’re struggling in this area or simply want a faster way to coordinate surgeries and book more cases, take a guided tour of HST’s scheduling & care communication.
Don’t miss out on the good stuff – Subscribe to HST’s Blog & Podcast!
Every month we’ll email you our newest podcast episodes and articles. No fluff – just helpful content delivered right to your inbox.