Vice President of Clinical Strategies
Patients are entitled to a copy of their medical records – always have been, always will be. This has caused some concern for clinicians though as those medical records contain their chart documentation, and that documentation can potentially lead to confusion, misunderstandings, and tension. Chart documentation can be short and curt, and while it may make sense to a healthcare professional, it might not make sense to a patient.
The Cures Act of 2020 only exacerbated these concerns and brought them front and center. The act dictates all health care facilities that use Electronic Health Records (EHRs), including Ambulatory Surgery Centers (ASCs), must provide the patient with free access to the patient’s medical record within a “reasonable” time.
So how do we go about meeting the patient’s and clinician’s needs?
Right off the bat, it may feel like we’re being forced to open a whole can of worms. But, once you’re comfortable sharing this chart documentation with patients, it will only lead to better patient care and communication.
Here are some practical charting tips for your clinical staff that will help them accurately describe the care provided without using words that will trigger, offend, or overwhelm patients and ultimately ease any concerns they have.
Cures Act 2020 – Patient Access
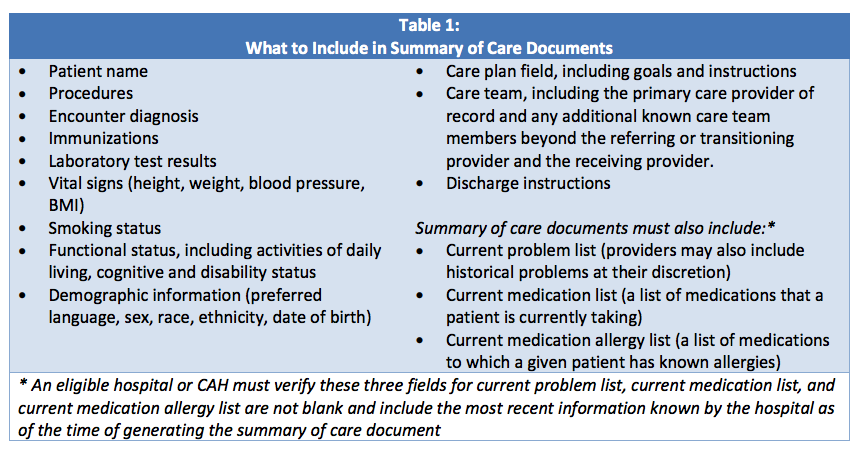
The Cures Act prohibits providers, developers, and health information exchanges (HIEs) from engaging in practices that inhibit patients from receiving their data or inhibit patient data from flowing where patients would like it to go. Patients have the right to free access to their records. The ASC record is usually short, and therefore providing the entire document is easily accomplished. At the very least, the system should export and print the summary of care information (see table below). Either way, the patient will have the names of their care providers and their assessment data.
Below is the list of Summary of Care Documents you should be prepared to send to patients as needed.
Best Practices
The bottom line is patients will see their chart, but there is no need to be afraid once you develop a few good habits. Here are a few best practices:
- Emphasize the importance of the patient having a strong sense of ownership over this information encourages a collaborative approach.
- Be factual, consistent, and accurate.
- Update the chart as soon as possible after any recordable event.
- When the patient gives the data in person, and it contains sensitive information, either put it in quotes or reword the information in a less inflammatory way.
- If the data populates from a patient portal, use their own words and confirm them where necessary.
- When it comes to sex/gender, be respectful yet clinical in your approach to this topic. When it is crucial to include disparate information, do so. If it isn’t, then don’t highlight this.
- If the data doesn’t fit in the box, make a new box.
Pitfalls to stay away from:
- Do not use words like obese. While we understand the clinical implications of this word, refer to the patient’s BMI when possible.
- Do not state a subjective assessment as fact. Include words like “observed” or describe what is assessed without personal conclusions. While you could say, “the patient seems afraid,” you might want to rephrase it as, “the patient was trembling, heart rate elevated, and states they ‘hate hospitals.’”
- If you are in the habit of saying the same thing for each patient (i.e., copy/paste), make sure the words fit the patient.
- If you are using paper charts, or at any time apply your signature, make sure it is legible. Patients tend to believe that clinical staff who confidently and clearly sign their notes are to be believed and will stand by the documentation.
Following these simple tips will result in less stress and more articulate, accurate documentation moving forward. Improved documentation will lead to better patient care and condition communication, better progress monitoring, clarity, consistency, and efficiency.
When you begin documenting on your next patient, take a few minutes to read your information through your patient’s eyes. It will quickly become your new standard.
Don’t miss out on the good stuff – Subscribe to HST’s Blog & Podcast!
Every month we’ll email you our newest podcast episodes and articles. No fluff – just helpful content delivered right to your inbox.

